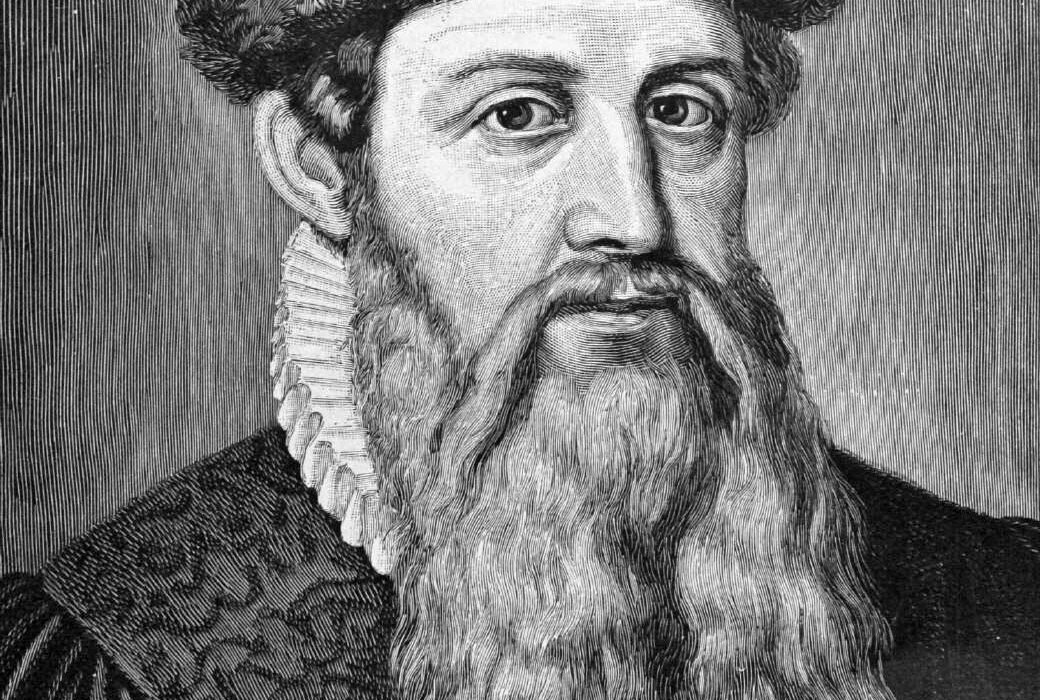
Joseph Lister (1827–1912) was a British surgeon and pioneer of antiseptic surgery, whose work revolutionized medical practice and greatly reduced the risk of infection during and after surgeries. Drawing on the germ theory of disease proposed by Louis Pasteur, Lister introduced the use of carbolic acid (phenol) to sterilize surgical instruments and clean wounds, drastically reducing postoperative infections. His methods, first implemented in the 1860s, marked a turning point in medical history, as they demonstrated that microorganisms were responsible for surgical infections and could be controlled. Lister’s antiseptic techniques transformed surgery from a high-risk procedure often leading to fatal infections into a safer practice, saving countless lives. His innovations earned him widespread recognition and helped lay the foundations for modern aseptic techniques used in hospitals today. Lister is often regarded as the “father of modern surgery,” and his legacy continues to influence medical practices worldwide.
Early Life and Education
Joseph Lister was born on April 5, 1827, in Upton, Essex, England, into a Quaker family known for its strong commitment to science and industry. His father, Joseph Jackson Lister, was a wine merchant and an amateur scientist who significantly contributed to the development of the achromatic lens for microscopes. This invention allowed clearer and more precise observations under the microscope, laying the groundwork for significant advancements in biology and medicine. Lister’s mother, Isabella Harris, was a devout Quaker who instilled in her children the values of hard work, humility, and service to others.
Growing up in a scientifically inclined household, Lister developed an early interest in science and medicine. His father’s work with microscopes had a profound influence on young Joseph, fostering a fascination with the microscopic world. He attended a Quaker school in Hitchin, Hertfordshire, where he excelled in his studies, particularly in the sciences. Despite his academic talents, Lister was known for being quiet and reserved, qualities that would follow him throughout his life.
After completing his primary education, Lister went on to study at Grove House School in Tottenham, London, where he continued to excel academically. His interest in medicine grew stronger, influenced by the scientific environment at home and his exposure to the works of pioneering scientists. In 1844, Lister entered University College London, one of the few universities in England that accepted Quakers at the time. He initially enrolled as a student of the arts but soon switched to medicine, drawn by a desire to understand the human body and alleviate suffering.
At University College, Lister studied under several prominent figures in medicine and science. One of his most significant mentors was William Sharpey, often referred to as the “father of British physiology.” Sharpey’s teachings in physiology and anatomy left a lasting impression on Lister and played a critical role in shaping his approach to medical research. Another influential figure in Lister’s education was Robert Liston, a renowned surgeon known for his speed and skill in the operating theater. Liston’s emphasis on surgical precision and his openness to new ideas would later resonate with Lister as he developed his antiseptic techniques.
Lister graduated with a Bachelor of Arts degree in 1847 and subsequently earned his Bachelor of Medicine and Master of Surgery degrees in 1852. His academic achievements were notable, but it was his meticulous approach to his studies and his keen interest in scientific inquiry that set him apart from his peers. During his time at university, Lister became increasingly aware of the high mortality rates associated with surgical procedures. Patients often succumbed to postoperative infections, a problem that perplexed the medical community and seemed insurmountable at the time.
After completing his medical education, Lister embarked on a tour of Europe, where he visited leading medical centers and studied under prominent surgeons and physicians. This journey broadened his perspective on medicine and surgery, exposing him to different techniques and practices. It was during this time that Lister first encountered the work of Louis Pasteur, a French chemist and microbiologist whose research on fermentation and microbial life would later play a crucial role in Lister’s development of antiseptic surgery.
Upon returning to England, Lister began his surgical career as a house surgeon at University College Hospital. His early experiences in the operating room were both challenging and eye-opening. He witnessed firsthand the devastating effects of postoperative infections, known as “hospital gangrene,” which claimed the lives of many patients. These experiences left a deep impression on Lister and fueled his determination to find a solution to this deadly problem.
Early Career and Research
In 1854, Joseph Lister moved to Edinburgh, Scotland, to work as an assistant to James Syme, a prominent Scottish surgeon known for his expertise in amputation and his innovative approaches to surgical procedures. Syme was a demanding mentor, but he recognized Lister’s potential and provided him with opportunities to develop his skills as a surgeon. Under Syme’s guidance, Lister honed his surgical techniques and gained valuable experience in the operating room. He quickly established himself as a skilled and meticulous surgeon, earning the respect of his colleagues and patients.
During his time in Edinburgh, Lister continued to grapple with the issue of postoperative infections. He was deeply troubled by the high mortality rates associated with surgery and the prevalence of conditions such as erysipelas, pyemia, and septicemia, which often led to death in patients who had undergone seemingly successful operations. These infections, known collectively as “hospitalism,” were poorly understood at the time, and there was little consensus among surgeons about their causes or how to prevent them.
Lister’s scientific curiosity and determination led him to investigate the underlying causes of these infections. He began conducting experiments and observations, meticulously documenting his findings. One of the key observations that Lister made during this period was the role of inflammation in postoperative infections. He noted that inflammation was often accompanied by the production of pus, which he believed was a sign of infection. This observation led him to theorize that the presence of “putrefaction” in the wound was responsible for the infections that plagued surgical patients.
Lister’s interest in the microscopic world, nurtured by his father’s work with microscopes, played a crucial role in his research. He began using the microscope to examine tissues and fluids from infected wounds, searching for clues that might explain the cause of postoperative infections. His microscopic studies revealed the presence of tiny organisms, which he believed were responsible for the process of putrefaction. However, Lister lacked a clear understanding of how these organisms caused infections, and his early theories were speculative.
Around this time, Lister encountered the work of Louis Pasteur, whose research on fermentation and the role of microorganisms in food spoilage provided a new perspective on the problem of surgical infections. Pasteur’s experiments demonstrated that microorganisms, or “germs,” were responsible for the fermentation of wine and beer, as well as the spoilage of milk. He also showed that these microorganisms could be killed by heat or chemical agents, a discovery that would later become central to Lister’s antiseptic techniques.
Inspired by Pasteur’s work, Lister began to explore the possibility that microorganisms were also responsible for the infections that occurred after surgery. He hypothesized that these germs entered the body through surgical wounds and caused the process of putrefaction, leading to the development of infections. This idea was revolutionary at the time, as the prevailing belief among surgeons was that infections were caused by “miasma” or bad air, rather than by living organisms.
To test his hypothesis, Lister began experimenting with different methods to prevent the entry of microorganisms into surgical wounds. He first focused on the use of chemicals to kill the germs present in the air and on surgical instruments. Lister experimented with various substances, including carbolic acid (also known as phenol), which had been used in the treatment of sewage. He reasoned that if carbolic acid could prevent the putrefaction of sewage, it might also be effective in preventing the putrefaction of wounds.
In 1865, Lister conducted his first successful experiment using carbolic acid to prevent infection in a surgical wound. He treated a young boy with a compound fracture of the leg, a condition that often led to severe infection and amputation. Lister applied a solution of carbolic acid to the wound, covered it with a piece of lint soaked in the acid, and then applied a bandage. To his satisfaction, the wound healed without any signs of infection, and the boy’s leg was saved. This success marked a turning point in Lister’s career and set the stage for his development of antiseptic surgery.
Development of Antiseptic Surgery
Building on his early successes, Joseph Lister continued to refine and expand his antiseptic techniques, transforming the practice of surgery and saving countless lives. In 1867, Lister published a series of papers in The Lancet detailing his experiments and the principles behind his antiseptic method. These papers, titled “On the Antiseptic Principle in the Practice of Surgery,” outlined the use of carbolic acid to sterilize surgical instruments, dressings, and the hands of surgeons, as well as to disinfect the air in the operating room.
Lister’s antiseptic method was based on the principle of preventing the entry of germs into surgical wounds. He emphasized the importance of cleanliness and the use of antiseptic agents to kill microorganisms that might cause infections. Lister’s approach involved several key steps: the application of carbolic acid to the surgical site, the use of sterilized instruments, the wearing of clean surgical attire, and the maintenance of a sterile environment in the operating room. He also advocated for the use of antiseptic dressings to protect wounds during the healing process.
The impact of Lister’s antiseptic method was profound. Within a few years, the mortality rate from surgical procedures began to decline significantly in hospitals that adopted his techniques. Lister’s work provided a scientific explanation for the causes of surgical infections and offered a practical solution to prevent them. His methods were initially met with skepticism by some members of the medical community, who were reluctant to abandon traditional practices and were wary of the use of chemical agents in surgery. However, as more surgeons began to adopt Lister’s antiseptic techniques and witnessed the dramatic reduction in postoperative infections, his ideas gained widespread acceptance.
One of the most significant aspects of Lister’s antiseptic method was its emphasis on the use of carbolic acid as a disinfectant. Lister believed that carbolic acid was effective in killing the germs that caused putrefaction and infection. He developed a variety of techniques for applying carbolic acid during surgery, including the use of carbolic acid sprays to disinfect the air in the operating room and the application of carbolic acid-soaked dressings to wounds. Lister also introduced the use of carbolic acid-soaked sutures for closing wounds, which helped reduce the risk of infection at the incision site. He meticulously tested and refined his methods, constantly seeking ways to improve the effectiveness of antiseptic surgery. For example, he developed a special carbolic acid spray apparatus designed to create a fine mist of the antiseptic in the operating room, aiming to kill airborne germs that might settle on the surgical wound. While this spray method was eventually deemed less effective than other techniques, it demonstrated Lister’s commitment to thoroughly exploring every avenue to reduce the risk of infection.
One of the key challenges Lister faced in promoting his antiseptic methods was overcoming the skepticism and resistance from the medical community. Many surgeons were entrenched in traditional practices and were reluctant to adopt new techniques, especially those that involved the use of chemicals like carbolic acid. Some of Lister’s contemporaries were initially critical of his work, arguing that the introduction of such strong chemicals could do more harm than good. Others questioned the validity of the germ theory of disease, which was still a relatively new and controversial concept at the time.
Despite these challenges, Lister was determined to prove the efficacy of his antiseptic techniques through careful documentation and dissemination of his findings. He published numerous articles and papers, detailing his methods and the outcomes of his surgeries. He also conducted public demonstrations and lectures, where he presented his antiseptic techniques to other surgeons and the broader medical community. These efforts gradually helped to win over skeptics and spread the adoption of antiseptic surgery.
Lister’s perseverance paid off as more and more surgeons began to recognize the value of his methods. Hospitals that implemented Lister’s antiseptic techniques reported significantly lower mortality rates among surgical patients. The reduction in deaths from postoperative infections was so dramatic that it became increasingly difficult for critics to dismiss the effectiveness of antiseptic surgery. Over time, Lister’s ideas gained widespread acceptance, and he became recognized as one of the foremost figures in the field of surgery.
By the late 1870s, Lister’s antiseptic methods had become standard practice in many hospitals across Europe and the United States. His work had not only transformed the practice of surgery but had also laid the foundation for the broader field of infection control in medicine. Lister’s emphasis on cleanliness, sterilization, and the prevention of infection would later influence the development of aseptic techniques, which sought to eliminate germs from the surgical environment altogether, rather than simply killing them with antiseptics.
Lister’s contributions to medicine were widely recognized during his lifetime. In 1869, he was appointed Professor of Clinical Surgery at the University of Edinburgh, a position that allowed him to continue his research and teach the next generation of surgeons. His reputation as a pioneering surgeon and scientist continued to grow, and he was invited to speak at medical conferences and institutions around the world. Lister’s antiseptic techniques were adopted by military surgeons during the Franco-Prussian War (1870-1871), further demonstrating their effectiveness in reducing the incidence of infection in traumatic injuries.
In addition to his work on antiseptic surgery, Lister made important contributions to the understanding of wound healing and tissue repair. He conducted experiments on the healing process of tissues, studying how different factors, such as the presence of infection or the type of suture material used, affected the outcome of surgical procedures. Lister’s research in this area helped to advance the field of surgical pathology and improved the outcomes for countless patients.
Challenges and Controversies
Despite the success of Joseph Lister’s antiseptic techniques, his work was not without its challenges and controversies. The adoption of his methods was met with resistance from some quarters of the medical community, and Lister faced significant obstacles in convincing his peers of the validity of his approach. One of the major challenges Lister encountered was the prevailing skepticism about the germ theory of disease, which underpinned his antiseptic techniques.
During Lister’s time, the germ theory was still a relatively new and contested concept. Many physicians and surgeons adhered to older theories, such as the miasma theory, which posited that diseases were caused by “bad air” or noxious vapors. This theory was deeply ingrained in medical practice, and the idea that tiny, invisible organisms could be responsible for infections was met with doubt and even ridicule by some of Lister’s contemporaries. Convincing the medical community to abandon the miasma theory and embrace the germ theory was a formidable task.
Another source of controversy was the use of carbolic acid itself. Some surgeons were concerned about the potential side effects of using such a powerful chemical on patients’ wounds. Carbolic acid, while effective at killing germs, could also cause irritation and damage to tissues if not used correctly. There were reports of patients experiencing burns or other adverse reactions to carbolic acid dressings, leading some to question the safety of Lister’s methods. Additionally, the carbolic acid spray that Lister initially advocated for use in the operating room was criticized for its harshness and potential to cause respiratory irritation among surgical staff.
Lister addressed these concerns by continuously refining his techniques and adjusting the concentration of carbolic acid used in his procedures. He was meticulous in his experiments, carefully monitoring the outcomes of his surgeries and making modifications as needed to improve the safety and effectiveness of his antiseptic methods. Lister’s commitment to scientific rigor and his willingness to adapt his methods in response to new evidence were key factors in the eventual success of his antiseptic techniques.
Despite Lister’s efforts to improve his methods and demonstrate their effectiveness, resistance to his ideas persisted in some circles. In particular, older and more established surgeons were often reluctant to change their practices, viewing Lister’s antiseptic techniques as overly complex or unnecessary. Some critics argued that the improvements in surgical outcomes observed under Lister’s care were due more to his skill as a surgeon than to the antiseptic measures themselves. Others dismissed the need for antiseptics altogether, believing that good surgical technique and proper hygiene were sufficient to prevent infections.
The controversy surrounding Lister’s work was not limited to the medical community. The public and the press also weighed in on the debate, with some newspapers publishing sensationalized accounts of the dangers of carbolic acid. Lister’s methods were sometimes portrayed as radical and experimental, and there were instances where patients or their families expressed concern about the use of antiseptics in surgery. These challenges highlighted the difficulties Lister faced in gaining widespread acceptance for his ideas, even as the evidence of their effectiveness continued to mount.
Despite these challenges, Lister remained steadfast in his commitment to advancing the field of antiseptic surgery. He continued to publish his findings and present his work at medical conferences, gradually winning over more and more supporters. His perseverance paid off, and by the 1880s, the tide had begun to turn in favor of antiseptic surgery. The growing body of evidence supporting the germ theory of disease, combined with the undeniable success of Lister’s methods in reducing surgical mortality rates, eventually led to widespread acceptance of antiseptic practices.
In recognition of his contributions to medicine, Lister received numerous honors and accolades during his lifetime. In 1883, he was made a baronet by Queen Victoria, and in 1897, he was elevated to the peerage as Baron Lister of Lyme Regis. These honors reflected the profound impact of Lister’s work on the field of surgery and his enduring legacy as a pioneer of antiseptic techniques.
Later Career and Honors
As Joseph Lister’s antiseptic techniques gained widespread acceptance, his reputation as a pioneering surgeon and scientist continued to grow. In 1877, Lister was appointed Professor of Clinical Surgery at King’s College Hospital in London, a prestigious position that allowed him to further develop and teach his methods. During his time at King’s College, Lister continued to refine his antiseptic techniques and expand their application to various types of surgical procedures. He also trained a new generation of surgeons in the principles of antiseptic surgery, ensuring that his methods would be passed down and adopted by future practitioners.
Lister’s work had a profound impact not only on the practice of surgery but also on the broader field of medicine. His emphasis on cleanliness, sterilization, and the prevention of infection helped to lay the groundwork for the development of aseptic techniques, which sought to create a completely sterile environment in the operating room. These techniques, which included the sterilization of surgical instruments, the use of sterile gloves and gowns, and the disinfection of the operating room, would become standard practice in the years following Lister’s death.
In addition to his contributions to surgery, Lister was also involved in various medical and scientific organizations throughout his career. He was a founding member of the British Medical Association and served as its president in 1896. Lister was also an active member of the Royal Society, one of the most prestigious scientific organizations in the world. In recognition of his contributions to science and medicine, Lister was awarded numerous honors and accolades throughout his life.
One of the most significant honors Lister received was his appointment as President of the Royal Society in 1895, a position he held until 1900. During his tenure, Lister played a key role in promoting scientific research and fostering collaboration between scientists and medical professionals. His leadership helped to strengthen the ties between the fields of medicine and science, further advancing the understanding of diseases and their treatment.
Lister’s influence extended beyond the United Kingdom, as his antiseptic techniques were adopted by surgeons around the world. His work had a particularly strong impact in the United States, where surgeons such as William Halsted and Harvey Cushing became strong advocates of antiseptic and aseptic techniques. Lister’s ideas also spread to continental Europe, where they were embraced by leading surgeons in France, Germany, and other countries. The global adoption of Lister’s methods helped to establish antiseptic surgery as a standard practice, leading to significant improvements in surgical outcomes and patient survival rates.
Throughout his later career, Lister remained committed to advancing the principles of antiseptic surgery and the broader field of medical science. Even as his methods gained widespread acceptance, Lister continued to explore new ways to improve patient outcomes and reduce the risk of infection. He was deeply involved in the development of aseptic techniques, which sought to eliminate the presence of germs in the surgical environment altogether, rather than merely killing them with antiseptics. Lister recognized that aseptic surgery, which involved sterilizing instruments, using sterile gloves, and creating a sterile operating environment, represented a significant evolution of his original ideas.
Lister’s influence on the field of surgery was profound, and his contributions extended well beyond the operating room. He was an advocate for the professionalization of surgery and the importance of rigorous scientific training for surgeons. Lister believed that surgeons should not only be skilled practitioners but also informed scientists who understood the underlying biological principles of their work. This approach helped to elevate the status of surgery as a scientific discipline and contributed to the development of modern surgical education.
In his later years, Lister continued to receive numerous honors and accolades in recognition of his contributions to medicine. In addition to his baronetcy and peerage, Lister was awarded honorary degrees from universities around the world, including Oxford, Cambridge, and Edinburgh. He was also elected as an honorary fellow of numerous medical and scientific societies, both in the United Kingdom and abroad. These honors reflected the global impact of Lister’s work and his enduring legacy as one of the most important figures in the history of medicine.
Despite his many accomplishments, Lister remained humble and focused on his work. He was known for his meticulous attention to detail and his commitment to patient care. Even as his fame grew, Lister continued to personally oversee surgeries and take a hands-on approach to teaching his students. He was deeply respected by his colleagues and students alike, not only for his scientific achievements but also for his dedication to the well-being of his patients.
In the later stages of his career, Lister’s health began to decline, and he gradually reduced his involvement in surgical practice. However, he remained active in the scientific community, continuing to attend meetings and contribute to discussions on medical and surgical advancements. Lister’s final years were marked by a growing recognition of his contributions to the field of surgery and the widespread adoption of his antiseptic and aseptic techniques in hospitals around the world.
Joseph Lister passed away on February 10, 1912, at the age of 84. His death was widely mourned, and he was remembered as a pioneering figure who had revolutionized the practice of surgery. Lister’s legacy lived on through the countless lives saved by the techniques he developed and the principles he championed. His work laid the foundation for modern surgical practice and infection control, and his influence can still be seen in operating rooms and hospitals around the world today.
Legacy and Impact
Joseph Lister’s contributions to medicine have had a lasting and transformative impact on the field of surgery and beyond. His pioneering work in antiseptic surgery not only revolutionized surgical practice but also fundamentally changed the way the medical community understood and approached the prevention of infections. Lister’s legacy is one of innovation, dedication to patient care, and a relentless pursuit of scientific knowledge.
One of the most significant aspects of Lister’s legacy is the widespread adoption of antiseptic and aseptic techniques in surgery. Before Lister’s work, surgery was often a last resort due to the high risk of infection and death. The introduction of antiseptic methods drastically reduced the mortality rates associated with surgical procedures, making surgery a safer and more viable option for treating a wide range of conditions. Lister’s work paved the way for the development of modern surgical techniques and the expansion of surgical procedures that were previously considered too dangerous to attempt.
The principles of cleanliness and sterilization that Lister championed have become fundamental to all areas of medical practice, not just surgery. Today, the importance of maintaining a sterile environment in healthcare settings is universally recognized, and infection control measures are a standard part of patient care. Lister’s influence can be seen in the protocols used in hospitals, clinics, and laboratories around the world, where the prevention of infection is a top priority.
In addition to his impact on surgical practice, Lister’s work also contributed to the broader acceptance of the germ theory of disease. Although the germ theory was still a contentious idea when Lister began his work, the success of his antiseptic techniques provided strong evidence in support of the theory. As more surgeons adopted Lister’s methods and saw the dramatic reduction in postoperative infections, the idea that microorganisms could cause disease gained credibility. This shift in understanding helped to propel advancements in microbiology, immunology, and public health.
Lister’s influence extended beyond the medical community to the general public as well. The success of antiseptic surgery and the growing awareness of the importance of cleanliness in preventing disease led to changes in public health practices. Efforts to improve sanitation, promote hygiene, and control the spread of infectious diseases were informed by the principles Lister had demonstrated in the operating room. These public health measures have had a profound impact on reducing the incidence of infectious diseases and improving overall health outcomes.
Lister’s legacy is also reflected in the institutions and organizations that continue to honor his contributions to medicine. Hospitals, medical schools, and research institutions around the world have been named in his honor, and numerous awards and lectureships have been established to recognize excellence in surgical practice and infection control. The Lister Medal, awarded by the Royal College of Surgeons of England, is one of the most prestigious honors in surgery and is given in recognition of outstanding contributions to the field.
Beyond the specific techniques and practices he introduced, Lister’s legacy is also one of a broader cultural shift in medicine. His emphasis on evidence-based practice, meticulous attention to detail, and commitment to improving patient outcomes set new standards for medical practice. Lister’s approach to surgery was not just about the application of antiseptics but about a fundamental rethinking of how surgery should be performed, with a focus on minimizing harm and maximizing the chances of a successful outcome. This approach has influenced generations of surgeons and medical professionals and continues to shape the practice of medicine today.
In reflecting on Lister’s legacy, it is clear that his contributions have had a far-reaching impact that extends well beyond the field of surgery. His work has saved countless lives and continues to inform the practice of medicine in ways that are still being felt today. Joseph Lister’s name has become synonymous with the principles of antisepsis and infection control, and his legacy is one of innovation, dedication, and a relentless pursuit of knowledge in the service of improving human health.